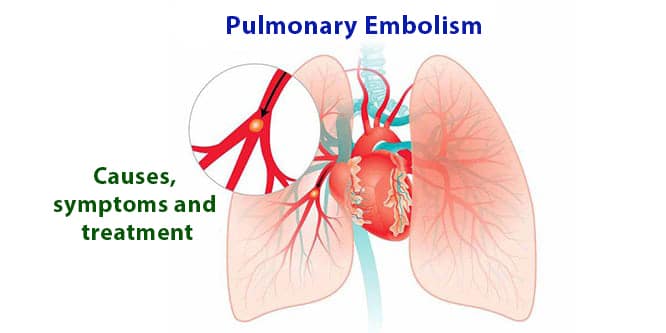
Pulmonary embolism is a condition arising from the sudden blockage of the pulmonary artery (which carries blood from heart to lungs) with clot and requires immediate medical help. Factors such as immobilization due to long lasting trips or being bedridden, or impaired vascular structure due to various reasons may increase the risk of pulmonary embolism. However, this condition may be prevented by taking some measures. Sudden onset shortness of breath, chest pain and cough are the most common symptoms. As these symptoms are not specific for this condition, diagnosis might be difficult. Unless immediately intervened, pulmonary embolism might be fatal. Main treatment methods include blood thinning medications, and if necessary, surgical intervention.
Table of Contents
What is pulmonary embolism?
Pulmonary embolism is a condition where a clot is formed in pulmonary artery and suddenly blocks it. It requires immediate intervention. It can completely occlude the main pulmonary artery, or its branches. The severity of embolism is based on the size of the blood clot and the patient’s coexisting diseases. As the blood flow to lungs is restricted by blood clot, blood cleaning function of lungs is diminished. The oxygen level of blood decreases, and this affects all organs. If the blood clot is multiple and very large, the condition might be fatal.
Causes of pulmonary embolism
Pulmonary embolism occurs due to a blood clot getting stuck in a pulmonary artery. Blood clots are usually formed in deep vessels of the body. This is also known as deep vein thrombosis. In this condition, blood clots are usually formed in legs or pelvis, and the reasons of blood clot formation include:
- Injury: Injuries including bone fracture or muscle ruptures caused by road accidents, surgical interventions or other traumas may damage the blood vessels, and this may lead to clot formation.
- Immobilization: When you stay immobilized for a long period of time, gravity slows down the blood flow of the bottom regions of your body. As a result, the risk of blood clot formation increases. Sitting through a long trip or being bedridden for a long time due to an illness may cause this.
- Medical conditions: Treatment methods including surgery or cancer chemotherapy may also cause blood clotting.
Risk factors for pulmonary embolism
- Medical history: If you have a personal or familial history of venous blood clots or pulmonary embolism, you are under a higher risk. In this case, you may have a genetic disorder which causes blood clotting.
- Heart disease: Certain heart diseases and heart failure increase risk of clot formation.
- Cancer: Pancreas, ovary, lung cancers and many other metastatic cancers as well as the chemotherapy administered for cancer treatment may increase the levels of substances that cause blood clotting. Women who have a personal or familial history of breast cancer and use tamoxifen or raloxifene are also under high risk.

- Tobacco use: Tobacco use may predispose individuals to blood clot formation especially when there are other risk factors present.
- Being overweight: Being overweight increases the risk of blood clotting especially in women who are smoking or have high blood pressure.
- Supplemental estrogen use: Estrogen in birth control pills and hormone replacement therapy may increase clotting factors in blood especially if you are smoking or overweight.
- Pregnancy: Pressure on the pelvic vessels due to fetus weight slows down blood flow from legs. When the blood flow is slowed down, possibility of clot formation increases.
Symptoms of pulmonary embolism
- Sudden onset and increasing shortness of breath
- Chest pain
- Cough
- Blood spitting with cough (Hemoptysis)
- Swelling, redness and pain in one leg
- Lightheadedness
- Sweating, unrest, fear of death
The severity of the symptoms of pulmonary embolism is based on size and place of blood clots, and whether patient has other conditions. The patient may have only one or all of these symptoms. If you notice one or more of these symptoms (shortness of breath), you should seek immediate medical help.
Chest pain in pulmonary embolism
Chest pain is knife-like and especially gets more severe with breathing. The individual may even need to stop halfway through their breathing due to chest pain. While the chest pain in heart attack is a pressing pain which is spread to arms; it is localized in pulmonary embolism. It does not spread to arms and the patient can easily locate the pain.
Diagnosis of pulmonary embolism
It is not always easy to diagnose pulmonary embolism. The above symptoms may be present in many conditions. For differential diagnosis of these symptoms, physical examination, and laboratory and imaging methods are used.
Physical examination
During physical examination, physician closely inspects your legs to check for swelling, tenderness, discoloration or temperature rise on your legs. These signs are very important as they may indicate that a clot is present in one of your vessels.
Blood tests
If pulmonary embolism is suspected, first test to be requested is D-dimer (clot breakdown product) level. If the result is normal, pulmonary embolism is ruled out. However, if result is high, further analyses are necessary to confirm diagnosis of pulmonary embolism. Blood tests can also determine the oxygen and carbondioxide amount in your blood. A clot in a pulmonary vessel will decrease the oxygen level of the blood. Additional blood tests can also be performed to determine whether you have a genetic clotting disorder.
Imaging tests
- Chest X-ray: It is not taken for the diagnosis of pulmonary embolism. It helps us diagnose other conditions which may be mixed up with pulmonary embolism.
- Electrocardiogram (ECG): It is colloquially known as heart graphy. This test measures the electrical level of the heart.
- Echocardiography (ECHO): It is the ultrasonography of heart. It shows the changes in the heart. It provides valuable information both for diagnosis and treatment.
- Doppler Ultrasound: It provides information whether there is clot in deep leg veins. Because pulmonary embolism is frequently accompanied by this condition.
- CT Angiography: It is the computerized tomography method performed by simultaneous contrast agent administration from the arm. It might be used for diagnosis as it shows the presence of clot in pulmonary arteries.
- Magnetic Resonance Imaging (MRI): This scan use radio waves and magnetic field to produce detailed images. It provides direct imaging of the clot in pulmonary arteries.
- Pulmonary scintigraphy: As it involves less radiation than the computerized tomography, it can be preferred in young women, pregnant women and patients with kidney disease. Its biggest disadvantage is the fact that it cannot be taken under emergency room condition.
- Pulmonary angiography: It is considered as gold standard test providing definitive diagnosis in pulmonary embolism. It is an expensive procedure using interventional technique which requires experience. So, it is not preferred much in clinical practice.
Treatment of pulmonary embolism
The treatment of pulmonary embolism should be initiated without delay. In fact, if the pulmonary embolism is suspected, the first dose of the medication to be used for the treatment should be administered. Treatment options may vary based on the severity of the condition and the patient’s coexisting conditions:
Medical treatment of pulmonary embolism
- Thrombolytic (clot-busting) treatment: It is used in cases who have fainting and low blood pressure. The aim is to prevent the heart from wearing down by busting the clot in pulmonary artery and restore the blood circulation to the lungs. However, there is a high risk of bleeding. Therefore, all kinds of risks are explained to the patient, and the treatment is initiated after benefit/risk calculation. Its effect starts to diminish after the first 7 days. Clot-busting treatment can be administered up to 14 days. It is not recommended to be continued beyond 14 days.
- Anticoagulant (clot prevention) treatment: It is initiated in patients with good clinical condition. These medications are colloquially ‘blood thinning’ medications. It is administered at therapeutic dose for 5 days, followed by a maintenance dose for long term treatment. The patient should be monitored closely during this period. If risk factors are present, the treatment should continue at least 3 months, if not, at least 6 months. Other treatments can be considered in case of worsening.
Surgery for pulmonary embolism
- Embolectomy: If clot-busting medication cannot be given to a patient with hemodynamic impairment due to the risk of bleeding or if the patient’s clinical condition does not improve after clot-busting medication, embolectomy (clot removal) is performed surgically or using catheter. Other than these, surgical treatment is also first option when a clot is detected in right cardiac cavities. Its biggest drawback is the fact that it cannot be performed in every center.
- Inferior vena cava filter: In some patients who cannot use medications due to high risk of bleeding or clot recurrence in lungs during treatment, inferior vena cava (main vessel collecting the blood coming from legs) filter is applied. Thereby, new clot formation can be prevented.
Supportive care
Oxygen support is provided to the patients with shortness of breath. If necessary, patients with shortness of breath can be hospitalized to intensive care unit. Supportive treatment to increase the blood pressure is initiated in patients with low blood pressure.
Is pulmonary embolism fatal?
Pulmonary embolism is a disease which requires fast diagnosis and treatment. The outcome might be dramatically different if the treatment is initiated early. The death rate in untreated patients is around 25-30%. In patients who started early and proper treatment, the death rate can be dropped to 2-8%. Death rate is usually higher in cases of cancer and chronic heart diseases, and elderly patients.
Complications of pulmonary embolism
The size of the blood clot and the patient’s health status play an important role in the outcome of pulmonary embolism. If blood clot is not completely dissolved, it might become chronic. In this case, “chronic thromboembolic pulmonary hypertension (CTEPH)” develops. If shortness of breath is worsening over time in patients suffering from pulmonary embolism, CTEPH must be considered.
Pulmonary embolism prevention
- If you are at risk for pulmonary embolism, you may need to use clot prevention medications before all surgical operations, mainly major surgeries.
- Mechanical measures including compression socks and pneumatic compression devices should be taken in bedridden patients.
- It is necessary to be mobilized as early as possible after an operation. Active exercises help muscles return into activities and leg veins activate.
- Avoid long-lasting trips if possible. If you have to, take frequent stopovers. Drink plenty of fluids during the trip.
- Exercise frequently and regularly as much as possible. You can prefer jogging, walking, swimming and cycling exercises.
- Be mindful about your weight as being overweight means an extra load for your heart and blood circulation in addition to your veins.
- Smoking cessation is necessary.
Herbal treatment for pulmonary embolism
As the treatment of pulmonary embolism is emergent, herbal treatments are not preferred for early treatment of condition. Some herbs might be detrimental if they interact with warfarin, a blood thinning (anticoagulant) medications. Herbal treatments can be used for protection against clots other than during critical stage.
Garlic
It is long known that garlic has a blood thinning property in addition to its many benefits. Regular garlic consumption may help prevent blood clots. However, if you are using blood thinning medications, consult with your physician about the amount of garlic you can eat. Its interaction with your medication might be detrimental.
Extra-virgin olive oil
A study published in American Journal of Clinical Nutrition has shown that phenol in olive oil decreases blood clot formation. Clotting might increase in individuals using animal oil in their diet.
Kiwi
It is not a secret that a diet rich in fruits and vegetables is good for heart health. However, researchers from University of Oslo have revealed that kiwi has an important place among these foods. The study has found that individuals who eat two or three kiwis a day have lower platelet activity, and thereby, a lower risk of blood clotting.
Do not use herbal products without consulting with your physician! Other than these, the following foods also reduce the risk of pulmonary embolism thanks to their blood thinning effect:
- Foods containing vitamin E and vitamin D (fruits, vegetables, organic eggs and some types of mushroom).
- Spices including turmeric, thyme, hot pepper and ginger
- Genuine black cacao
- Fruits like papaya, strawberry and pineapple
- Crude honey
- Apple cider vinegar
- Green tea
- Fish oil and omega-3 fatty acids obtained from wild-caught fish
- Beans, legumes, nuts, seeds, fish and range-fed meat
Be sure that you take sufficient amount of fluid by drinking herbal teas or water. Avoid excessive sugar, alcohol or coffee use.
Does pulmonary embolism recur?
There is a recurrence rate of 5-23% despite treatment. The period in which the recurrence is most common is within the first 6-12 months after treatment. Caution should always be taken for this.
Recommendations for pulmonary embolism patients
- Inform yourself about your condition using proper sources. The greatest side effect of the medications is the risk of bleeding. In case of a bleeding (e.g., nosebleed), you must seek help from emergency room.
- Drink plenty of water unless there is a health reason not to. Thereby, your body does not get dehydrated, and fluidity of the blood does not get impaired.
- As the treatment may last for 3-6 months and sometimes even longer, treatment adherence is very important. The medications must be used without missing even one dose.
- As pulmonary embolism may recur, seek immediate medical help in case of sudden onset chest pain, shortness of breath and cough.
- Follow-up visits must not be missed. If you have a new or worsening symptoms, you must inform your physician.
- Patients suffering from pulmonary embolism can continue with their daily lives provided that they comply to treatment. Also check:>>> Pulmonary Embolism,